NASHVILLE — Captain Christopher Kroboth, MS, NRP, CCEMT-P, from the Fairfax County Fire and Rescue Department/Virginia Commonwealth University (VCU) Paramedic Program, credits the effective use of active simulation in a flipped training program as instrumental to providing students with “a rolodex of experience” to help them enhance sensory cues to recall past learning experiences, resulting in better patient care.
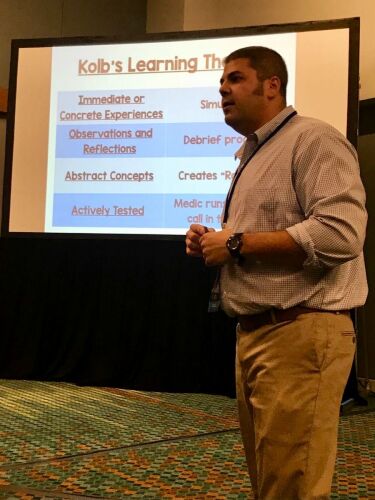
In a session at EMS World Expo, Kroboth discussed the benefits of combining the flipped classroom model with sensory cues, active simulation and stratified debriefings to empower students to take ownership of their education and training.
Memorable quotes on active simulation in training and education
Here are some of memorable quotes from Kroboth on active simulation in education and training.
“We need to engage their learning.”
“We have to create those stressful environments for them to recall.”
“During a debrief, when students get that live feedback from their peers, it’s powerful.”
Top takeaways on active simulation in training and education
Traditional lecture-style classrooms are getting a new look in some foundational paramedic programs. Using scenario-based education in a flipped classroom environment, Kroboth and his team of educators have empowered their students to take control of their learning experience.
The results: better medics, which leads to better patient care. Here are some top takeaways from this session.
1. Effective learning goals
When educators set out to teach, their goals are to provide quality, cost-effective training designed to increase student productivity and enrichment. Kroboth’s program is set to accomplish these goals to create an effective learning environment by:
- Active student engagement
- Fostering learning through participation
- Role play
- Emotional experience
- Full sense immersion (i.e., sight, smell, touch and sound)
2. Students storing data and recalling it when needed
In a traditional classroom setting, paramedic students are set up to receive a lot of data in a short amount of time. The ability to process this data allows students the capability to respond to emergency situations, assess a patient’s condition and render the appropriate care.
Kroboth poses a question: what happens when students have the ability to store the data but are unable to process this information into action during moments of increased stress?
He credits the blank stare and inability to respond to students’ inability to connect with recalling past experiences. Under stress, the brain looks for common experiences to help drive decision-making and action. Inexperienced students will have nothing to recall, thereby making it difficult to respond to the patient’s needs.
Active simulation and debriefing allows his students to build a “a rolodex of experience” which enables them to recall past experiences more quickly and accurately under stressful situations.
Lieutenant Christopher Kroboth, MS, NRP, CCEMT-P, from the Fairfax Virginia Commonwealth University (VCU) Paramedic Program, discussed the benefits of combining the flipped classroom model with sensory cues, active simulation and stratified debriefings to empower students to take ownership of their education and training.
3. Using sensory in simulation training
As a medic, it is important to use your senses (sight, smell, touch and sound) to help gather patient information, assess their needs and render adequate treatment. As an instructor, it is important to stimulate these senses during real-time scenarios to help students remain focused in their environment, patient and tasks, Kroboth noted.
4. Self-reflection and stratified debriefing
Technology advances are responsible for creating a constant need for stimulation in today’s students. This can be a challenging for some educators whose teaching style is unidirectional with linear communication.
Kroboth uses principals from David A. Kolb’s Experiential Learning Theory to design a learner-centric process using cognitive and behavioral stimulus that assist learners in thinking about:
- What they did
- How they did it
- How they can improve
Using a 20-10-20 format during scenarios, teams are able to interact with 20 minutes of real-time scenarios, including students in role-play as the patient and bystander that is recorded. The response crew then takes 10 minutes of self-reflection as a crew to do a team hot wash, and 20 minutes of a stratified debrief with the instructor starting by asking “so walk us through your call.”
The end-goal of learning through debrief is designed to:
- Make it effective
- Make it experiential
- Make it learner – centric
- Make it count
- Make it real
Learn more about active simulation training
Learn more about active simulation EMS training with these articles from EMS1:
- Dozens of tips for EMS educators and training officers
- Quick Clip: Pros and cons of the flipped classroom model
- Virtual EMS education: Growing pains and lessons learned
- Pediatric simulation training: Tips to make it effective for medics
- 3 ways to teach capnography with active learning
- 3 important considerations for simulation debriefing
- 4 patient assessment scenarios that are actually useful for EMS students
- 6 tips for debriefing EMS simulation scenarios
- 7 Questions to keep paramedic students on track during simulation
- 10 tips to maximize learning in lab scenarios
References
- Herreid, C., & Schiller, N. (2013, May). Case Studies and the Flipped Classroom. Journal of College Science Teaching, 42(5), 62-66.
- Chall, J. S., & Adams, M. J. (2002). The academic achievement challenge: What really works in the classroom? New York: Guilford Press.
- Al-Ghareeb, A. Z., Cooper, S. J., & Mckenna, L. G. (2017). Anxiety and Clinical Performance in Simulated Setting in Undergraduate Health Professionals Education: An Integrative Review. Clinical Simulation in Nursing, 13(10), 478-491. doi:10.1016/j.ecns.2017.05.015
- Murray, Adam. “Mind the gap: technology, millennial leadership and the cross-Generational workforce.” The Australian Library Journal, vol. 60, no. 1, 8 July 2013, pp. 54–65., doi:10.1080/00049670.2011.10722556.
This article was originally posted Nov. 6, 2018. It has been updated.













