 |
| Download the ARDS Algorithm from Univ. of Mich. Survival Flight (PDF) |
A critical care transport team is called to the intensive care unit of a small community hospital for a 44-year-old, 70 kg female who is post-operative, day two, from an elective laparoscopic cholecystectomy. She was unable to wean from mechanical ventilation following surgery and a cystic and hepatic vessel leak was found on abdominal CT. Based on CT and clinical and laboratory findings, the patient was diagnosed with acute pancreatitis. Her chest X-ray revealed diffuse pulmonary infiltrates and atelectasis, consistent with Acute Respiratory Distress Syndrome.
Current ventilator settings include a tidal volume (Vt) of 650 ml, respiratory rate of 30 breaths/minute, PEEP of 18 cmH20 and 100 percent of fiO2. Peak inspiratory pressures are reading 60 cmH20 and oxygen saturation is reading 81 percent. Is this adequate support for this patient? Are these ventilator settings appropriate? How should the transport team proceed?
ARDS
According to the National Heart, Lung, and Blood Institute’s (NHLBI) ARDS Network: Acute Respiratory Distress Syndrome (ARDS) is a devastating, often fatal, inflammatory disease of the lung characterized by the sudden onset of pulmonary edema and respiratory failure, usually in the setting of other acute medical conditions resulting from local (e.g. pneumonia) or distant (e.g. multiple trauma) injury.
These patients are some of the most challenging cases that air medical transport personnel will be tasked with delivering to tertiary care. Understanding current ventilator strategies as well as your own program’s capabilities and limitations will improve chances for a successful transport and patient outcome.
ARDS is characterized by the entry of protein-rich fluid into the air spaces due to increased alveolar-capillary permeability. As a result, ventilation-perfusion (V/Q) mismatch and physiologic “shunting” cause hypoxemia. Increased physiologic dead space may interfere with CO2 elimination and increased minute ventilation is required to maintain normal CO2 levels in the blood.
In the ARDS patient, much of the lung is so consolidated that it can’t be recruited to participate in gas exchange. This is especially true in the dependant regions of the lung. Since only a small amount of the lung participates in ventilation during ARDS, it has been conceptualized as a “baby lung” (this is in contrast to the original “stiff lung” theory). As a result, less affected lung regions must accommodate for most of the Vt. This can result in regional over-inflation and Ventilator Associated Lung Injury (VALI).
A great deal of study has been dedicated to effective ventilation strategies of patients with ARDS. Current treatment goals include maximizing oxygenation as well as protecting injured lung area in order to allow healing. Ensuring that the clinician is not accomplishing one goal at the expense of the other is often the challenge in the critical care setting.
Protective-Lung Ventilation
For patients with ARDS, Vt and respiratory rate are set to meet ventilatory requirements and limit VALI associated with alveolar over-distention. Per the protective lung ventilation strategy, 6 ml/kg tidal volume and a plateau pressure (pressure seen by the alveoli) of no more than 30 cm H20 should be maintained, regardless of mode of ventilation (ARDS network recommendations). The goal for adequate lung recruitment and a higher PO2 may be achieved with increased positive end expiratory pressure (PEEP) and a lower Vt. If the patient experiences “breathe stacking” (occult PEEP due to inadequate expiratory time, often referred to as “Auto PEEP”) or a plateau pressure less than 20 cm H2O, Vt may be increased to a maximum of 8 ml/kg, as long as plateau pressure remains below 30 cm H2O (NIH National Heart Lung and Blood Institute).
Of particular interest with respect to mechanical ventilation is the ALVEOLI study. Completed in 2002, this randomized, controlled, multicenter clinical trial involved 861 patients and compared a Vt volume ventilatory strategy (6 mL/kg predicted body weight, plateau pressure less than 30 cm H2O) with a higher Vt (12 mL/kg predicted body weight, plateau pressure less than 50 cm H2O). This study was based on current clinical and experimental evidence suggesting that ventilation with high Vt and high pressures might be harmful to the injured lung. The results of this particular trial revealed an in-hospital mortality rate of 40 percent in the 12 mL/kg group and 31 percent in the 6 mL/kg group — a 22 percent reduction. Ventilator-free days and organ-failure-free days were also significantly improved in the low Vt group. This ventilation strategy has been commonly referred to as “Protective Lung” ventilation. For more information on this ventilation strategy, visit http://www.ardsnet.org/node/77465.
Open-Lung Ventilation
This ventilation strategy protects lungs and minimizes VALI by reducing the amount of cyclical stretch on the alveoli. By keeping terminal lung units open longer, through utilization of PEEP and inversed inspiratory to expiratory (I:E) ratios, mean airway pressure (mPaw) is increased and there is more surface area for gas exchange. Ultimately, oxygenation should improve.
ARDS is not a homogeneous process. Different areas of the lung may require varied inflation times in order to ventilate. Functional alveoli are recruited more quickly than diseased or consolidated ones. Prolonging inspiratory time may recruit more of the lung to participate in gas exchange by giving diseased units more time to open.
Peak inspiratory pressures (PIP) are kept as low as possible while attempting to keep alveoli open. Driving pressure — measured as the difference between plateau pressure and PEEP — is kept below 20 cm H20 and PIP is limited to 40 cm H20 ideally. PEEP is usually kept between 10 and 20 cm H20. I:E ratios are kept at a maximum of 2:1. Ventilator rate should be limited to 30 breaths/minute. This is an uncomfortable method of ventilation for the patient and may require significant sedation and possibly neuromuscular blockade in order to maximize oxygen delivery and minimize oxygen consumption.
This strategy is not without risks. The high pressure required to open terminal lung units increases intrathoracic pressure. This in turn increases the risk of air trapping, barotrauma, and decreased cardiac output. Closely monitoring ventilatory and hemodynamic parameters is critical.
Issues for Air Medical Personnel
One challenge that air medical transport personnel face when applying current evidence-based practice to treatment plans, is that much of the research utilized applies mainly to bedside practice and not the unpredictable setting of the transport environment. This challenge is clearly evident when attempting to safely transport a patient with severe ARDS to definitive care. Circumstances beyond our control often force us to slightly modify the treatment plan originally developed in the intensive care unit.
Increased oxygen consumption and demand naturally occurs in any patient due to stresses of flight, altitude changes and patient movement. This is often a consequence that a patient with severe ARDS cannot afford. While protecting the lungs remains a primary goal during transport, we must attempt to compensate for the increased hypoxia that these patients often experience.
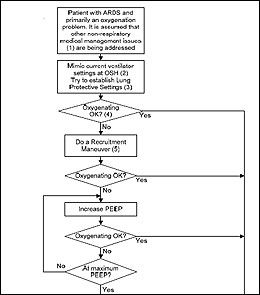
The ventilation strategies previously discussed are often not mutually exclusive in the transport environment. Increasing PEEP, inversing I:E ratios, manipulating respiratory rate to improve minute ventilation, and adjusting cabin altitude are often strategies used in combination to improve the oxygen delivery to consumption ratio. The following algorithm, collaboratively developed by The University of Michigan critical care staff, respiratory care department and Survival Flight offer an approach to treatment and transport of these complex patients.
| Download the ARDS Algorithm from Univ. of Mich. Survival Flight (PDF) - 107 KB |
References
- Brower RG et al. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. The New England Journal of Medicine 342 (18); May 4, 2000 (1301-1308).
- Slutsky AR and Tremblay LN. Multiple System Organ Failure: Is Mechanical Ventilation a Contributing Factor? Am J Respir Crit Care Med 157(6); 1998 (1721-1725).
- Burns SM. Mechanical Ventilation of Patients with Acute Respiratory Distress Syndrome and Patients Requiring Weaning: The Evidence Guiding Practice. Critical Care Nurse 25(4); August 2005 (14-24).
- Papadakos PJ and Lachmann B. The Open Lung Concept of Alveolar Recruitment Can Improve Outcome in Respiratory Failure and ARDS. The Mount Sinai Journal of Medicine 69(1&2); January/March 2002 (73-77).
- Amato MBP et al. Effect of a Protective-Ventilation Strategy on Mortality in the Acute Respiratory Distress Syndrome. New England Journal of Medicine 338(6); 1998 (347-354).
- http://www.ardsnet.org/. NIH National Heart Lung and Blood Institute. Accessed January 11, 2008.


