Having worked as a burn nurse in a critical care burn unit, I can attest that burn injuries are among the most devastating around. They’re painful, require long recovery time and can be disfiguring. This series will provide the firefighter and EMT with the basics of identification of burns and management of patients, as well as focusing on prevention issues that can help to decrease the number of burns in your community.
The number of such injuries is staggering. In the United States and Canada, there are more than 1.55 million burn injuries annually, which is about 4,300 per day. Each year, 950,000 patients visit emergency departments with burn injuries and 60,000 are hospitalized.
Burns are the second leading cause of accidental death, behind vehicle crashes, in children ranging from 1 to 4 years of age. Additionally, burns are the leading cause of injury and death for those aged 1 to 18 years.
Managing patients
The first rule for managing burn patients is to stop the burning process. For the first responders, it is common to arrive on scene and find the patient wrapped in blankets or some other type of cover. This can keep the heat trapped and further increase the burning process.
Cool the burn immediately with cool water to reduce the skin temperature, stop the burning process, numb the pain and prevent or reduce swelling. Do not use ice on burns as it may decrease the blood supply to the area and may actually make the burn worse.
Remove burned clothing, metal from belt buckles, etc, as these things can continue to burn if they retain heat. Loosen or remove tight clothing, jewelry and boots before swelling occurs. If the burn covers more than 30 percent of the total body surface area, you may have swelling in areas remote from the burn due to fluid shifts, so remove everything that might be constrictive.
After cooling the burn with water, cover the area with a clean dressing. Do not use a towel since the fiber can stick in the wound and be painful to remove. It is important to keep the burn victim warm as their thermoregulation may be disrupted. Be careful when cooling the burn that you do not cool the patient into a hypothermia state.
Determining extent of burned area
One of the cardinal rules when working with burn patients is to never underestimate the severity of a burn. It takes approximately 24 hours for a burn to fully “declare” itself regarding its severity. When treating burn patients, the provider should be able to determine the extent of the burned areas.
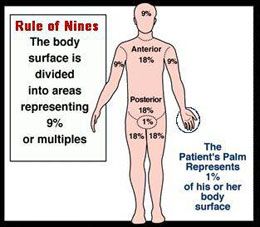
The easiest way to determine the amount of area burned is by using the “Rule of Nines.” This formula is easy to remember and accurate. As you can see from the graphic below, the body surface is broken down into areas representing 9 percent or multiples. A rule of thumb is that the patient’s palm represents 1 percent of their body surface area.
 |
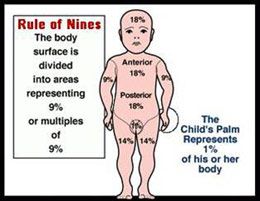
It is important to remember that there is a difference between the surface area of an adult and that of an infant/child; specifically, a child’s head is larger and their legs smaller compared to adults..(Interestingly, this difference in children changes their center of gravity and is why they fall over easier than older people.) When it comes to burns and children, keep in mind that youngsters are always reaching and pulling things. Children’s burns often happen when they pull a hot liquid, such as coffee or a pan of hot liquid, onto themselves. This can lead to scald burns on their heads and upper torso; burns to the head area of a child will result in a greater surface area of a child being injured when compared to the head of an adult. Understanding this is important to ensure an accurate determination of burned areas.
 |
When determining the extent of burns, remember that the patient may have a combination of second and third degree burns. This is important in providing the receiving hospital with the involvement of the burns, giving staff time to prepare for the patient.
Types of burns
The most common type of burn is a first degree burn. These are often caused by sun exposure. In some cases, these may develop small blisters that appear after a couple of days. Any blisters often break because of the fragile thin layer of skin involved. These burns, and any broken blisters, will need to be kept clean and the patient will need to remain well hydrated. The burns normally heal themselves within two weeks.
Second degree burns are more difficult to diagnosis because they present with a wider range of characteristics. Second degree burns can be either superficial or deep. They can often appear to be a first degree burn, and these are considered superficial. Because of the thickness of the skin involved and increased damage, these burns will have immediate blistering and also have a moist appearance. The blistering occurs when the epidermis is lifted from the dermis and filled with fluid.
Second degree burns are a very painful burn because the nerve endings in the skin are preserved. This is not the case with a third degree burn where the nerve endings are destroyed.
The other type of second degree burn is called either deep partial thickness burns or deep second degree burns. The appearance of these burns can vary, but often have a white and waxy surface. They can appear to be more serious than a third degree burn because of their appearance and the associated pain that comes from it. These burns usually take a longer time to heal, and often leave scarring. Deep partial thickness burns may require skin grafting to heal for the best results.
Third degree burns are the most serous type of burn because of the significant amount of the damage to the skin. They can vary in appearance with a range of colors such as white, red or brown. Unlike second degree burns, third degree burns are dry and often leathery or hard. The hardness is because the burning process has destroyed all the structures of the skin which give skin is elasticity. This includes damage to the support structures, such as the elastic fibers and collagen. The blood in the vessels has coagulated from the heat, resulting in no supply of blood to the area. The nerves have also been burned so there is no pain with this type of burn.
Third degree burns will not be able to heal on their own, except for very small burns. Because of the damage to all parts of the skin and supporting structures, there is no way that new skin will be able to form. These patients will need skin grafting and long-term medical care.
Treatment
When treating the patient, it is important to at least:
1. Ensure the burning process has stopped
2. Assess airway, breathing and circulation, as with any trauma patient
3. Evaluate the extent and percentage of burns
4. Treat any other associated injuries
5. Determine if fluid resuscitation is needed
While the first four have been discussed — and the order is important from both a safety and patient care issue — fluid resuscitation will have a separate column devoted to it later.
Care tips
To close the article, let’s sum up things:
- Second degree burns will have blisters that form immediately and appear moist. While a first degree burn does produce immediate blisters, they can appear later.
- One of the easiest methods to differentiate a second and third degree burn is the presence of site pain with a second degree burn.
- The patient’s palm roughly represents 1 percent of their body surface area. This can be useful to determine the area of a burn.
- The surface area is different between infants and children when compared to adults. An infant’s head has more body surface area than that of an adult.
- Remember that Stop, Drop, and Roll is not just for kids. Adults and firefighters need to keep this rule in mind if they ever catch fire.
- Train for the event of a firefighter on fire during training evolutions.
Burns are devastating injuries and we need to prepare to handle these quickly. The education can be as simple discussing the care issues over coffee, or incorporating them into training. Station officers owe this to their crew and the community they protect.
The next article in this series will discuss fluid resuscitation with the burn patient and prevention issues.

