Patients in severe respiratory distress or respiratory compromise are often unable to speak more than one or two words at a time, and attempting to do so makes their distress even worse. Use these eight yes-no questions to learn from the patient about their medical history and present illness. These questions are the start of a conversation to guide treatment decisions. With a calm voice, explain to the patient that you need them to nod or shake their head — yes or no — to these questions:
1. Has this happened before?
Most patients in severe respiratory distress have a chronic condition that exacerbates; meaning it can get worse. If the answer to this question is yes, look at the patient, scan the room, and start naming out loud the most likely culprits. For a younger patient seated next to a nebulizer, start by asking if this is an asthma attack. For an older patient seated next to an ashtray, ask if this is from their COPD. With a patient who woke up in the middle of the night next to a box of blood pressure medications, ask if their current respiratory compromise is from heart failure.
If the answer is no to those likely culprits, consider the acute causes that fit the patient’s age and appearance. These include flash pulmonary edema from an acute myocardial infarction, pulmonary embolism, pneumothorax or anaphylaxis.
2. Have you ever been this bad before?
Follow by asking if they have ever been intubated for breathing difficulty before, and if they felt this bad when that happened. This helps you anticipate the need to assist their ventilation with a bag-valve-mask device or place an advanced airway, and will help the ED staff determine the course of treatment.
3. Ask if a specific treatment worked for this before
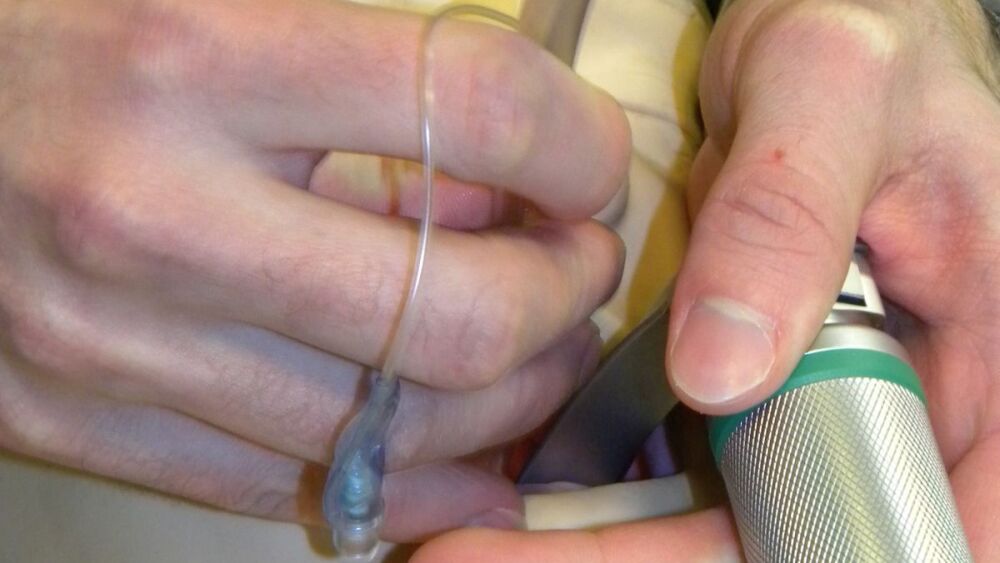
Many patients with asthma, COPD and congestive heart failure put off calling 911 until after home treatments have failed. An asthmatic who has not gotten better after using albuterol is likely to need more than just albuterol from you. Start naming your available treatment options and ask they if they worked in the past. Use terms they can understand, such as a “pressure mask” for CPAP, “shot of epinephrine,” or “magnesium through an IV.”
4. Did your breathing difficulty start right before you called 911?
Use this question to determine the onset of symptoms. If the patient shakes their head “no,” follow up with times when their respiratory distress began. Did it start 30 minutes before calling? An hour? Three hours? All night? This, along with what the patient has done for home treatment before you arrived, also helps predict the need for assisted ventilation with a bag valve mask.
5. Did this episode come on suddenly?
This question helps narrow down the cause if it is not known yet. If the answer is yes, clarify by asking if the patient felt completely normal before having trouble breathing. A sudden onset is more evidence of an acute cause — asthma, MI, anaphylaxis, pulmonary embolism, or pneumothorax. A gradual progression of symptoms suggests a COPD exacerbation or pneumonia.
6. Do you have pain anywhere? If yes, point where
If the patient points to their chest, follow up with more yes-no questions to identify a cardiac component. Does it feel like a pressure? Is it sharp? Does it get worse when you breathe? Does it move anywhere? Sharp pain that gets worse with inspiration suggests musculoskeletal chest pain, and pressure that does not change with inspiration and radiates suggests a cardiac cause. Chest and leg pain with difficulty breathing may be from a pulmonary embolism. For any patient with chest pain, follow up on these questions with a 12-lead ECG after managing their airway.
7. Are you getting tired?
Patients in respiratory distress can decompensate to respiratory failure from the ongoing effort needed to breathe, even if they are able to inhale enough oxygen to maintain an adequate pulse-ox reading. A patient who nods “yes” to this question is not getting better, and is likely to need assisted ventilation with a bag valve mask soon. These patients often close their eyes, have difficulty holding a nebulizer to their mouth, or difficulty holding their head up. Prepare a BVM and airway equipment, and work on a plan with team members.
If a patient shakes their head “no,” ask if they feel like they are getting better. If the answer is yes, this indicates that your current treatment is working, and reporting this to the emergency department may prevent them from getting intubated. If the patient is improving try asking open-ended questions to see if they can tolerate speaking in longer phrases, and for them to describe their symptoms.
8. Are there any medications you can’t take?
Ask this question to identify medication allergies. If the patient answers yes but cannot communicate what it is, start by asking about antibiotics. They are among the most common medications people are allergic to, and many patients with difficulty breathing receive antibiotics in the hospital. Attempt to identify which medication and report it to the hospital.
These questions provide a starting point for the assessment of respiratory compromise. Combine the questions with lung sound auscultation, pulse oximetry and waveform capnography to guide treatment. A capnography waveform with a slurred “shark fin” upstroke is diagnostic of bronchospasm, which provides immediate feedback on when albuterol should be administered to a patient who is unable to speak in phrases or sentences.
For patients in severe respiratory distress, make every question count. Ask yes-no questions that yield the most information, and ask the questions in ways that require the least amount of effort from patients in respiratory compromise.
Listen for more
Serial killers: Shortness of breath
In this episode, learn the 5 emergent conditions that will kill patients experiencing shortness of breath, and how to use ETCO2 to develop a differential
This article, originally published on Feb. 9, 2016, has been updated.