By Kevin T. Collopy
As prehospital medicine transitions from an industry of “rapid transport,” to that of delivering evidence-based medicine that improves patient outcomes, the time is now to address an often debated topic: whether or not antibiotics have a place in prehospital care.
Simply, the answer is yes.
In select and targeted patients, early antibiotics are proven to reduce both morbidity and mortality. Unfortunately, there are many states where EMS regulations prohibit the administration of prehospital antibiotics. These rules are dogma and are not based on current evidence.
The most commonly given reasons for prohibiting prehospital antibiotics is the risk of anaphylaxis – an allergic reaction to the medication - and that transport times are too short to provide a benefit. To this notion, Mayfield presented a research abstract which demonstrated that the most commonly indicated prehospital antibiotics (for sepsis) carried an allergic reaction rate of well under 1 percent.[1]
Furthermore, few drugs are given to patients within five minutes of ambulance arrival at an emergency department. It is true that transport times are often less than 20 minutes, however when you’re waiting another 15 minutes or more for an emergency department bed, the delays from first medical contact to antibiotic administration rise rapidly.
When considering adding antibiotics to any EMS system’s protocols, it is important to consider the following:
1. Understand when to administer prehospital antibiotics
Antibiotics are indicated for the prevention and elimination of bacterial infections. Not all infections are caused by a bacterial pathogen. Fungal, viral and parasitic infections can all present similarly to bacterial infections.
Two patient populations - those with known wounds that penetrate the fascia and those with severe sepsis - are most likely to benefit from prehospital antibiotics are. Patients with wounds extending below the fascia have had the deep internal structures of their skin exposed to the environment. In trauma centers, 100 percent of these patients later require surgical debridement and 100 percent receive a broad spectrum antibiotic, often 1-2 grams of IV cefazolin.[2] In patients with open fractures, early antibiotics have been demonstrated to reduce a patient’s infections risk by over 40 percent![3]
Sepsis is an infection cascade that will most likely worsen without intervention. Early in sepsis care, when a patient’s vital signs and lactic acid are stable, emergency departments will take time to wait for the results of blood cultures to determine which organism-specific antibiotics to administer and by which route. However, when hypotension or lactic acidosis develops, patient outcomes are improved by initiating two broad spectrum IV antibiotics within 60 minutes of initial patient contact.[4]
2. Understand when to withhold antibiotics
Equally important to understanding when to administer antibiotics, is understanding when antibiotics are not indicated. It is tempting when carrying a few antibiotics to administer them to all infections. This is dangerous!
In most instances it is paramount to wait until an infection is confirmed as bacterial in nature and then the type of bacteria determined. Only after these two questions are answered are patients given antibiotics specific to the infecting bacterium. Consider a patient with a suspected pneumonia or urinary tract infection; both of these may be treated by up to 10 different antibiotics depending on the identified organism.
3. Have targeted training
Antibiotics are another drug to know the dose, route, and time; it is important to know the contraindications, precautions, drug incompatibilities and side effects. In fact, these considerations are arguably more important than most other drugs carried on ambulances because there are many drugs such as dopamine, dobutamine, and furosemide that are incompatible with antibiotics. Some drugs have rather common side effects, such as Redman’s syndrome during vancomycin administration where flushing across the chest and head is frequently seen.
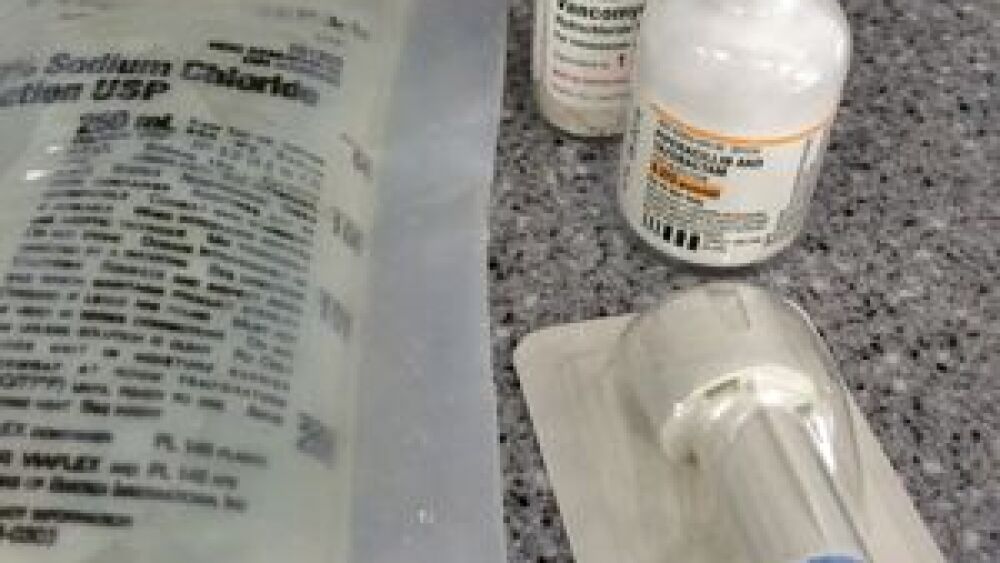
In addition, nearly all antibiotics require mixing prior to administration. Proper mixing is important so that the patient gets the proper dose. Whenever training for prehospital antibiotic administration, plan on an initial and annual training sessions on drug pharmacology, preparation, handling and administration.
4. Establish a monitoring system
Collaboration with all receiving hospitals for 100 percent utilization review of prehospital antibiotic administration is critically important. This two-way collaboration not only builds a close working relationship, but it also promotes patients’ safety. Consider creating arm bands to alert emergency departments of prehospital antibiotic administration; doing so helps to prevent double drug administration and alerts the emergency department leadership to which patients require follow up. Follow up on patients’ records for both appropriate prehospital indications as well as hospital diagnoses.
Several EMS systems across the United States are already administering prehospital antibiotics successfully. Recently, the EMS Systems in Greenville S.C., a healthcare system with four different receiving hospitals, began administering antibiotics to patients with symptoms of severe sepsis. Their goal is to demonstrate that administration is safe and effective before recommending their severe sepsis protocol be adapted state wide. It’s time all systems begin discussing the role targeted antibiotics have in their protocols as these drugs are safe and effective when administered to the right patients.
About the author
Kevin Collopy is the clinical education coordinator at AirLink/VitaLink Critical Care Transport in Wilmington, NC. He has been in EMS for over 15 years and has worked as a volunteer, in municipal 911, and in critical care transport. He is a well-known educator who regularly presents at regional and national conferences and is a textbook, eLearning course, and magazine author who serves on the IAFCCP Board of Directors.
References
1. Mayfield, TR, Meyers, M., Mackie, J, Incidence of Adverse Reactions to Initial Antibiotic Administration in Severe Sepsis Patients, poster presentation, EMSToday 2015 Baltimore, MD February 26, 2015
2. Antrum, RM and Solomkin JS, A Review of Antibiotic Prophylaxis for open Fractures, Orthop Rev 1987 Apr; 16(4): 246-54
3. Thomas SH, et al., Helicopter emergency medical services crew administration of antibiotics for op[en fractures, Air Med J 2013 Mar-Apr;32(2):74-9
4. Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19): 1,368–77, Nov 8, 2001