Clinical pearls of physical restraints
- Use the least amount of force possible when restraining any patient, but especially patients with increased ICP.
- Sedatives should be considered.
- Law enforcement must be on board the ambulance during transports of arrested persons with handcuffs applied.
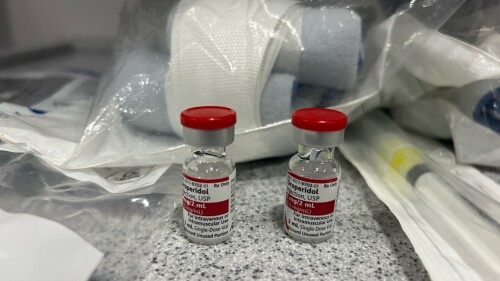
Clinical pearls of chemical restraints
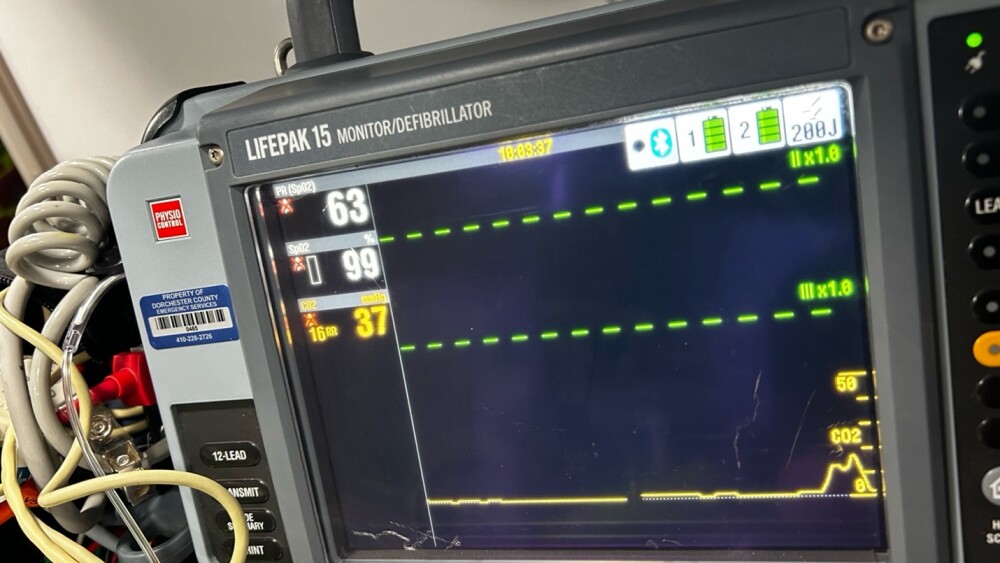
- Advanced airway equipment and cardiac monitoring must be available if a patient is to be given chemical restraints.
- If a patient’s respiratory status declines, ALS providers must be able and willing to take over the airway to prevent hypoxia.
Prehospital medicine, by its very definition, occurs in an imperfect and potentially dangerous environment. While the vast majority of prehospital encounters occur without incident, some situations necessitate EMS providers gain rapid control of patient behavior to protect the safety of the public and the patient.
The decision to provide prehospital agitation management involves heavy consideration of the patient’s rights, clinical status and the necessity of prehospital intervention in the first place.
What is patient agitation, really?
Agitation is a catch-all term for any form of general uncooperative state or aggressive behavior by a patient. It is a broad spectrum and ranges from verbal aggression to physical violence.
Agitation is most likely to require specific management when the patient’s behavior has begun posing a threat to themself, the community at large or the EMS providers tasked with their care. Examples of moderate-to-severe agitation include physical strikes toward EMS providers, self-injurious behavior or repeated attempts to remove vital, life-sustaining equipment, such as an ETT post-arrest.
Causes of patient agitation
When addressing agitation, it is important to ask why the patient is agitated in the first place. Underlying medical issues are often the cause for a patient’s agitation. For instance, patients who are delirious secondary to sepsis are unlikely to benefit from heavy sedatives and pharmacological intervention; rather, reversing their underlying acidosis and hypoperfusion will be the most beneficial.
Alternatives to physical and chemical restraints
Verbal counselling and de-escalation are always the gold standard of agitation management. Verbal patient coaching must be tailored to the specific patient and scenario that EMS clinicians are dealing with. A 20-year-old male in college is likely to require different therapeutic communication measures than an 80-year-old woman who is upset EMS is removing her from her nursing home room.
When employing verbal counselling, remember the patient is an individual with their own reasons for being agitated. If you can reverse the reason for their agitation and address their concerns, they are likely to be more cooperative. We are never trying to be punitive with agitation management.
Physical restraints
Examples of restraint methods include cravats (triangular bandages) and commercial restraint devices. A rolled sheet can also be tied around the patient’s extremities as needed. Commercial restraint devices pose the least risk to the patient and are often the simplest to apply.
In addition, it is critically important to avoid restraining patients in the prone position. Patients in the prone position are at severe risk of positional asphyxia. A 2021 study found that patients restrained in the prone position have decreased cardiac output in addition to a significantly, dangerously reduced tidal volume [9]. Hogtying patients or bending the extremities backward is not an acceptable practice and risks harm to the patient.
Restraints are not without risk. Excessively tight restraints pose the risk of neurovascular compromise and damage. Perform full CMS (circulation, motor, sensory) checks of each extremity prior to and following application of restraints. Guidelines from 2021 allow for two finger breadths within each restraint to avoid compromising circulation [3]. The NAEMSP position paper on restraints recommends against the use of hard restraints, such as handcuffs [3].
Head injury victims are at increased risk for elevated intracranial pressure (ICP) concerns. The act of restraining them is likely to induce further agitation and confusion. In doing so, we risk elevating ICP further and exacerbating the issue. Use the least amount of force possible when restraining any patient, but especially patients with increased ICP.
Law enforcement interactions
It is never acceptable to sedate or restrain a patient solely based on law enforcement direction. Always perform your own comprehensive assessment of the patient’s status and weigh the benefits to the risks of sedation and restraint use.
A patient who is handcuffed and under arrest must have law enforcement physically on the ambulance. Law enforcement must be readily available to release the patient’s handcuffs if the patient’s status declines.
Chemical restraints
Advanced airway equipment and cardiac monitoring must be available if a patient is to be given chemical restraints. Many of the common agitation medications carry a significant risk of respiratory depression. If a patient’s respiratory status declines, ALS providers must be able and willing to take over the airway to prevent hypoxia.
End tidal CO2 monitoring (ETCO2) is especially important for monitoring sedated patients. ETCO2 capnography allows providers to see a real-time waveform of the patient’s respirations and assess their rate, quality and the presence of carbon dioxide retention. Sedated patients are at increased risk for hypoventilation, which will in turn induce carbon dioxide retention and potentially lead to respiratory acidosis. If this occurs, the patient may require ventilatory support.
Pulse oximetry is another important vital sign to assess but often has a delay when showing changes in patient status. It is also significantly less reliable for patients with darker skin complexions [1].
Video: Treating agitated patients
References
1. Al-Halawani, R., Charlton, P., Qassem, M., & Kyriacou, P. A. (2023). A review of the effect of skin pigmentation on pulse oximeter accuracy. Physiological Measurement, 44(5), 05TR01. https://doi.org/10.1088/1361-6579/acd51a
2. Golparvar, M., Saghaei, M., Sajedi, P., & Razavi, S. S. (2004). Paradoxical reaction following intravenous midazolam premedication in pediatric patients - a randomized placebo controlled trial of ketamine for rapid tranquilization. Paediatric Anaesthesia, 14(11), 924–930. https://doi.org/10.1111/j.1460-9592.2004.01349.x
3. Kupas, D. F., Wydro, G. C., Tan, D. K., Kamin, R., Harrell, A. J., & Wang, A. (2021). Clinical care and restraint of agitated or combative patients by emergency medical services practitioners. Prehospital Emergency Care, 25(5), 721–723. https://doi.org/10.1080/10903127.2021.1917736
4. Lingamchetty, T. N., Hosseini, S. A., & Saadabadi, A. (2023, June 5). Midazolam. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537321/
5. Olejarczyk, J. P., & Young, M. (2022, November 28). Patient rights and ethics. StatPearls NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/portal/utils/pageresolver.fcgi?recordid=660f5efd72b48f442b428a43
6. Rahman, S., & Marwaha, R. (2023, September 1). Haloperidol. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560892/
7. Rosenbaum, S. B., Gupta, V., Patel, P., & Palacios, J. L. (2024, January 30). Ketamine. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470357/
8. Sicari, V., & Zabbo, C. P. (2023, July 10). Diphenhydramine. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK526010/
9. Steinberg, A. (2021). Prone restraint cardiac arrest: A comprehensive review of the scientific literature and an explanation of the physiology. Medicine, Science and the Law/Medicine, Science and the Law, 61(3), 215–226. https://doi.org/10.1177/0025802420988370