The first time I heard about Wernicke’s encephalopathy was October 17, 1994. I know that because I have a habit of dating classroom notes, as if they might expire a week or two later.
That Monday evening, I was two months into paramedic school, trying to keep up with pharmacology. The seventh of 21 drugs on the agenda was thiamine, also known as Vitamin B1. In my hurried scrawl, next to thiamine’s dose (100 mg) and indications (AMS, DTs), I wrote, “Admin before D50 to help metabolize glucose” followed by “Warnikey(?).” The question mark was to remind me I was guessing at the spelling, a consequence of the professor’s Midwestern twang that made diseases sound less German.
By the end of the lecture, I still had no idea what “Warnikey” was, but at least I knew what to do with thiamine. Or did I?
What is Wernicke’s Encephalopathy?
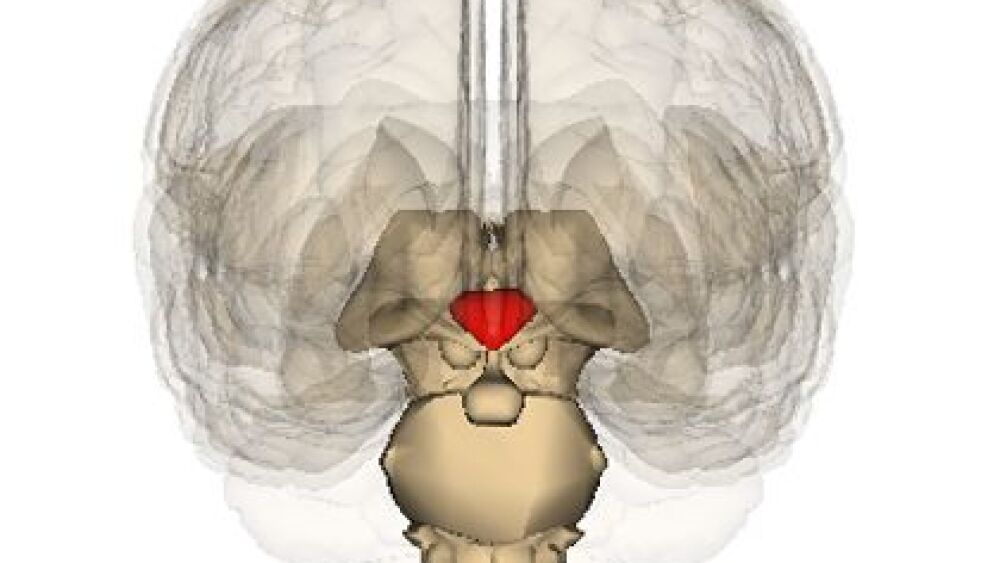
Wernicke’s encephalopathy is an acute neurological condition caused by thiamine deficiency, also known as beriberi. The disease affects the thalamus and hypothalamus and usually presents as confusion, loss of coordination (ataxia), and visual disturbances such as rapid eye movements (nystagmus) and double vision (diplopia). Long-term alcoholics are at greater risk for Wernicke’s encephalopathy because they don’t absorb thiamine well, but any condition causing malnutrition, such as anorexia, Crohn’s disease, chronic infection and gastric bypass, can lead to thiamine depletion.
Thiamine: 100 mg, 500 mg or zero mg?
It’s true that the antidote for WE is thiamine; however, that 100-mg dose we had to memorize is sub-therapeutic for many patients. Definitive care for WE is usually several 500-mg boluses of IV thiamine over the first 24-48 hours before tapering to 100 mg of oral medication daily.
Another misunderstanding about thiamine is that presumed alcoholics must be targeted for that vitamin more emergently than other hypoglycemic patients. Yes, thiamine is needed to metabolize sugar, and long-term alcohol abusers are more likely than others to be thiamine deficient, but it’s unrealistic to assume chronic ETOH abuse is always evident in the field. Classic signs of inebriation such as slurred speech, poor coordination and an alcohol-like odor can be caused by other etiologies, while many true alcoholics show no signs at all of their disease.
Besides, alcoholics aren’t the only ones at risk for thiamine depletion; so are infants, the elderly, pregnant women and patients on furosemide or digoxin, to name a few. And beriberi can present with systemic signs and symptoms unrelated to WE. Heart failure, nausea, sleep disturbances and irritability are just a few consequences of insufficient Vitamin B1.
There’s a 24-hour window from onset of WE until permanent damage is likely, but death from profound, untreated hypoglycemia occurs much more quickly — within an hour or so. Since blood glucose can be checked easily in the field while B1 levels cannot, it’s widely considered reasonable to administer dextrose without thiamine prehospitally, then transport patients for further evaluation.
At my last EMS agency, we didn’t even carry thiamine. I wondered if we were behind or ahead of the curve, so I took an informal survey of large EMS organizations like the ones in New York City, Nashville and Chicago. Only two of the 10 systems I checked still include thiamine in their protocols. At only $10-15 per 100-mg dose, it’s not the cost of the drug, but its perceived value that’s limiting prehospital use.
A fate worse than Wernicke’s
Say your semiconscious diabetic wakes up after a dextrose bolus and refuses transport. A repeat episode of low blood sugar isn’t the only risk that patient is taking.
As discussed, Wernicke’s encephalopathy is a short-term, reversible consequence of thiamine deficiency, but what happens when WE isn’t treated within its 24-hour window? About 20 percent of those patients become comatose and die. Most of the rest develop Korsakoff’s psychosis: permanent damage to the parts of the brain involving memory. Retrograde amnesia, inability to form new memories, confabulation and hallucinations are the most common signs and symptoms.
Korsakoff’s psychosis isn’t curable; sufferers are permanently handicapped and often require ongoing supervision. I remember one Korsakoff’s patient whose family tried caring for her at home. They force-fed her through a nasogastric tube and tried to prevent her from seeking alcohol, but she ended up in a hospital and died of multiple-organ failure.
WE and KP are often grouped together in the literature as Wernicke-Korsakoff syndrome. You might hear the disease referred to nonchalantly as “wet brain,” but there’s nothing casual about its toll on victims and their families. Prehospital providers should be aware of Wernicke-Korsakoff although most of us will never play a role in preventing it.
Works referenced
1. Bowman J. Thiamine before glucose, where’s the science? The Resuscitationist. www.resuscitationist.com. Accessed 11/06/16.
2. Alzheimer’s Association. Korsakoff Syndrome. www.alz.org. May 2016.
3. Lanska DJ. Korsakoff’s Psychosis. Encyclopedia of the Neurological Science. Elsevier, 2014.
4. Sanders MJ. Paramedic Textbook: Second Edition. Mosby, 2001: 1025-1030.
5. Hsieh A. Drunk versus diabetes: How can you tell? www.ems1.com. 07/31/11.