Editor’s note: The EKG Detective will be a monthly column dedicated to illustrating the benefits of utilizing deductive logic as a method for interpreting ECG tracings. The column will highlight and review all the basic ECG interpretations, before transitioning into a monthly interpretation challenge. See you next month and remember, it is always better to practice as a clinician rather than a technician.
Welcome back to the EKG Detective. This column is dedicated to illustrating the benefits of utilizing deductive logic as a method for interpreting EKG tracings. For this month’s article, we will be looking at premature atrial contractions (PACs).
If you need a refresher on inductive and deductive logic, check out our introductory article.
Fill out the form on this page to download your copy of the EKG Detective Interpretation Checklist.
Throughout this series, we will be using the EKG Detective Interpretation Checklist (see Figure 1). This checklist is intended to prompt providers through five sequential elements associated with basic EKG interpretation while working through the specific criteria for each element:
- Rhythm regularity
- Rhythm rate
- P-wave criteria
- PR interval
- QRS criteria
EKG rhythms will be eliminated as we identify criteria within the EKG tracing until there is only one probable interpretation. We will use this checklist to illustrate how deduction is used to interpret an ECG tracing. More practically, it can be used as an EKG interpretation job aid.
Atrial tachycardia
For this article, we will be looking at atrial tachycardia to illustrate the principle behind the EKG Detective (see Figure 2 for examples of atrial tachycardias). Atrial tachycardia originates somewhere within the atria, but not within the sinoatrial (SA) node. This is important to note because atrial foci do not have rate limitations that are typically associated with the SA node. Although the SA node can accelerate into the mid-to-upper 100 beats per minute, it is not designed to sustain those rates for extended periods of time. As a byproduct, atrial tachycardias tend to beat faster than a tachycardia originating from within the SA node.
EKG Category 1: Rhythm regularity
- Atrial tachycardia is characterized by a regular rhythm.
- As atrial tachycardia is regular, we should eliminate any rhythm that is irregular.
- We can also eliminate ectopic beats because they will cause the rhythm to be irregular (see Figure 3).
EKG Category 2: Rhythm rate
- Atrial tachycardia is associated with rapid ventricular rates. The ventricular rates typically fall between 150-250 beats per minute. The SA node can beat this fast, but it is not capable of sustaining rates above 150 beats per minute for long periods of time.
- As atrial tachycardia has a rapid rate, we should eliminate any rhythm that is not faster than 150 beats per minute (see Figure 4).
EKG Category 3: P-wave criteria
- Rapid ventricular rates cause R-to-R intervals to be squeezed closer together. Due to this squeezing, P-waves may be difficult to identify and/or isolate because they can be obscured by the T-waves.
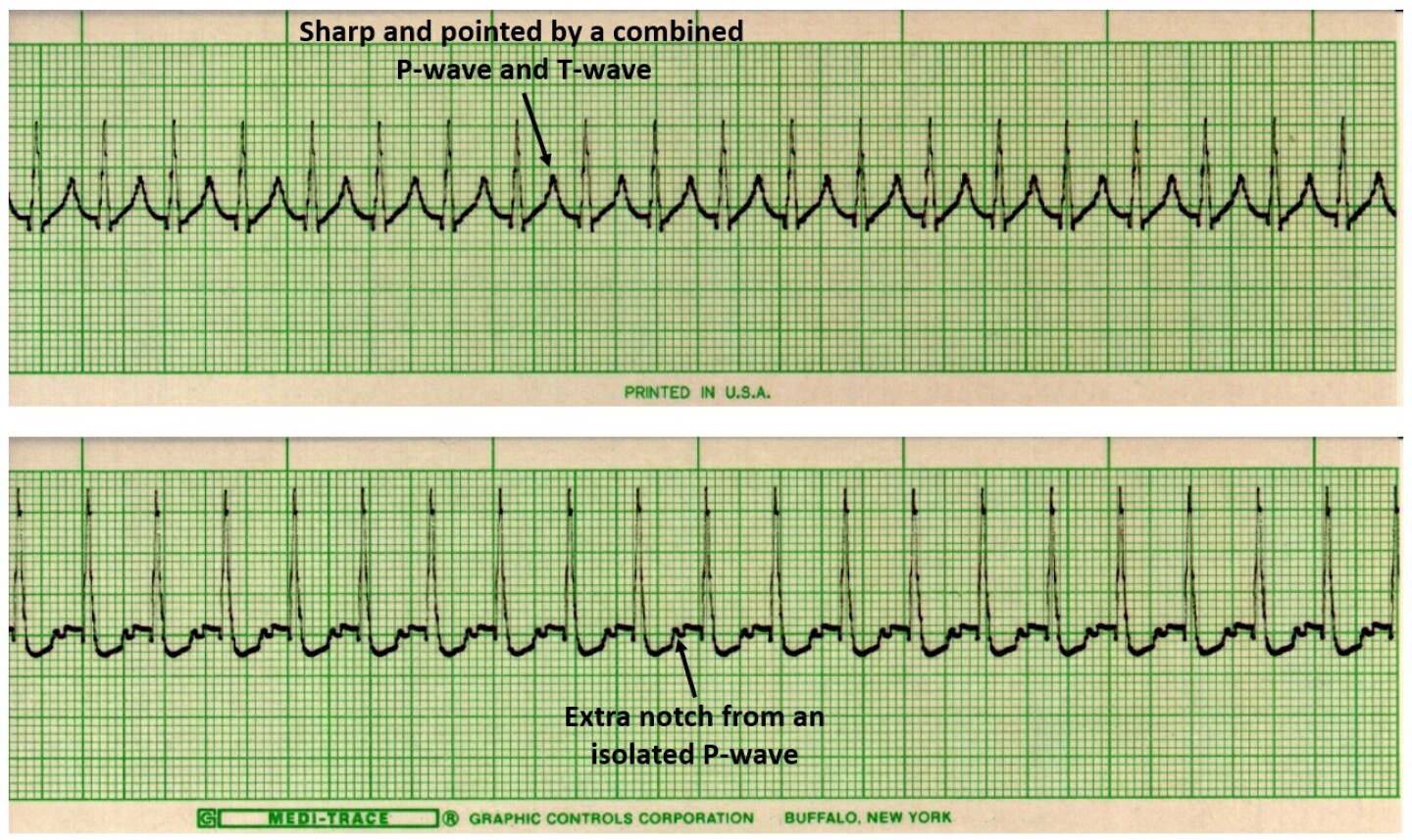
- Depending upon the timing of these wave forms, the combined P-waves and T-waves may appear sharp and pointed. If the T-waves have a pointed morphology, this is a good indication there is P-wave activity combining with the T-wave (see Figure 5).
- In some cases, you might be able to identify and isolate P-waves. This is done by identifying an extra notch within the T-wave. This is caused by the P-wave and T-wave intervals being squeezed together because of the increased rate (see Figure 5).
- Atrial tachycardia does not present with flutter waves, so we can eliminate atrial flutter (see Figure 6).
- There are not three or more different looking P-waves, so we can eliminate wandering atrial pacemaker (see Figure 6).
- There is not than one P-wave for every QRS complex, so we can eliminate heart blocks (see Figure 6).
EKG Category 4: PR interval
- As mentioned, P-waves can be difficult to identify and/or isolate. Because of this difficulty, measuring the PR interval may be a challenge. If the PR interval is measurable, it will typically measure between 0.12 to 0.20 seconds (see Figure 7).
- If the PR interval measures between 0.12 to 0.20 seconds, we can eliminate junctional tachycardia, because the interval for this rhythm will be less than 0.12 seconds (see Figure 8).
- There is no need to move onto EKG Category 5: QRS criteria, because the only remaining choice is the Atrial Tachycardia we have been working from.
Identifying atrial tachycardia
This illustrates how deductive logic is used to interpret atrial tachycardia. Atrial tachycardias tend to beat fast. The ventricular rate consistently beats at over 150 beats per minute. Remember to focus on the T-wave because it may appear sharp and pointed, or you might be able to identify the extra notch from an obscured P-wave.
See you next month, and remember, it is always better to practice as a clinician, rather than a technician.