About this series: Best Practices commissioned Jay Fitch to write a 12-part series on how EMS agencies and fire departments can adapt to the extreme pressures to operate more efficiently while exploring entirely new paradigms of how prehospital care can be delivered. He uses the concepts of organizational agility to provide a blueprint for the “strategic management of uncertainty.” The graphic above shows the four dimensions of organizational agility and the 11 factors impacting agility; each installment of this column will examine a different factor through the prisms of the four dimensions.
Fitch serves on the Best Practices editorial board of advisers and is a founding partner of Fitch & Associates, which has provided strategic and operational consulting services to EMS and the fire service for nearly three decades. To see the previous installments of this column, along with an agility self-assessment tool, visit fitchassoc.com/agility.
— Keith Griffiths, editor in chief 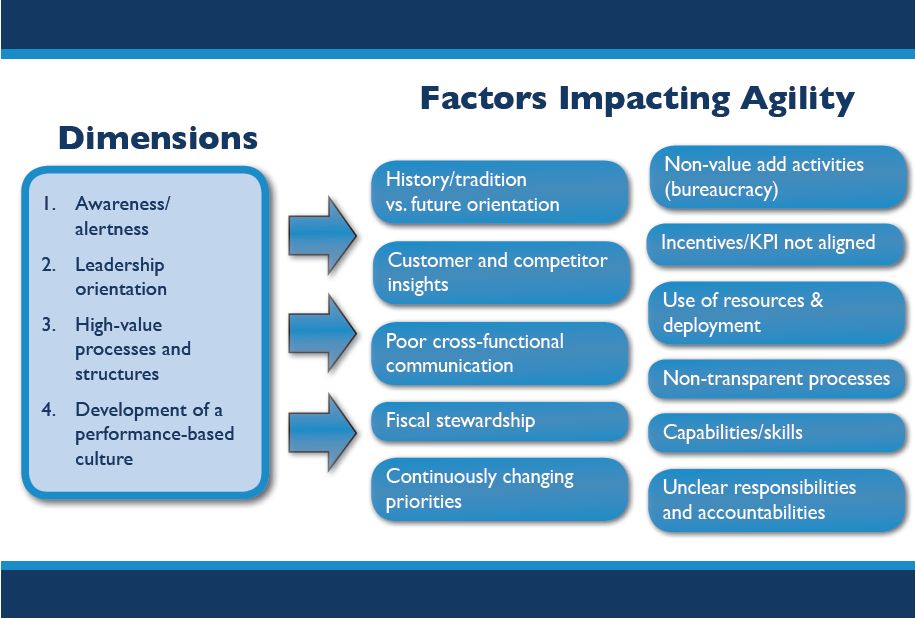 Early in my career, an ambulance owner I worked with decided to increase productivity by implementing a $1 incentive per completed non-emergency transport. This quickly became known as the “buck a body” program.
Early in my career, an ambulance owner I worked with decided to increase productivity by implementing a $1 incentive per completed non-emergency transport. This quickly became known as the “buck a body” program.
As you might imagine, the unintended consequence was that in the rush to collect their transport bounty, caregivers hurried through their duties, provided less care and were less than polite to customers. Clearly there was no alignment between improving a key performance indicator (productivity) and the actual result (loss of customers).
Let’s take a look at the difficult task of measuring key performance indicators (KPIs) and aligning appropriate incentives through the prisms of the four dimensions of organizational agility.
Awareness and alertness
In the early years of modern EMS, no one worried about measuring fractile response time targets, unit hour budgets, satisfaction levels and such things. We were focused on “healing the sick and raising the dead.” Everybody loved the medics! However, through the years, our ability to impress community and clinical leaders without metrics and measurement has been eroded.
Some EMS organizations were in tune with the times as the political landscape changed: They evolved and embraced performance measurement and improvement. Others continued to exhibit a “we’re the good guys and gals” approach, expecting—and even self-righteously demanding—their community’s support. One chief told me, “We don’t need to report our fractile response times every month. Council is happy with averages.” Without taking a breath, he went on to say, “The county’s medical control staff are making our lives miserable. They want to review each and every one of our patient refusals. It’s ridiculous—I have no idea what all the reasons are that patients refuse transport!”
Agencies that are alert to the changing environment become more agile while those that are arrogant and self-righteous become increasingly fragile. Measuring KPIs and aligning appropriate incentives for clinical, operational and financial performance is central to becoming more agile.
|
Leadership orientation
If the boss doesn’t “get it,” success in aligning incentives to support improved performance is nearly impossible. Early metric-driven incentives were generally focused on the financial aspects of the EMS organization by either claiming to increase profit margins or reduce costs. They were not always successful; driving down costs would sometimes come at the expense of quality, turnover and lost expertise—or even losing some of your customer support or market.
Fragile organizations today remain primarily focused on financial incentives rather than using a more balanced approach that includes aligning process improvement, customer satisfaction, and learning and development of those within the organization. These four pillars are the basis of today’s modern “Balanced Scorecards.” Scorecards gained notice 20 years ago after an article was published in the Harvard Business Review, and they have become a well-accepted way to report performance on KPIs today.
Current research suggests that world-class organizations are 159 percent more likely to have mature Balanced Scorecards in place than less successful organizations. And a 2008 study published in Advances in Accounting found that among 164 publicly traded organizations, those with well-deployed Balanced Scorecards outperformed the control group by nearly 30 percent.
It’s clear that leaders who are focused on the future and who can align multiple levels of incentives, appropriately matched to the generational specific motives of caregivers, encourage agility and outperform fragile leaders who are focused on the past.
High-value processes and structures
Agile EMS organizations understand that the Balanced Scorecard is an effective way to organize important processes to both measure and report performance. Put simply, “If you measure it, you can understand it. If you understand it, you can improve it.”
To be better understood and improved, EMS processes can be organized along classic scorecard dimensions:
-
Financial performance: Revenues, net earnings, return on capital, cash flow/days in accounts receivables, etc.
-
Customer value performance: Market share, customer satisfaction measures, including compliments, service inquiries and customer loyalty
-
Internal business process performance: Productivity rates, quality measures, response times throughout the organization
-
Employee performance/development: Morale, knowledge, turnover, best practices use
-
When working with clients, we suggest that for each high-priority process, they need to deeply understand the current state based on quantifiable operational data, using process maps and analysis to help identify major gaps between present and desired performance levels. It’s a bit tricky because the stated issue isn’t always the real problem.
For example, in a community we recently worked with, it became clear that the stated “employee out of chute time” issue was a system problem with several root causes. The time stamp was occurring at an incorrect interval and the station configuration (crew quarters at the back of the station on the second floor) impacted the ability to reasonably perform. In this case, response times by crew were posted, with top-performing crews receiving recognition at monthly caregiver meetings. With consistent reporting, recognition and reinforcement, competition between crews led to an overall response time improvement. The incentive in this case was recognition and positive reinforcement.
Development of a performance-based culture
An EMS organization’s ability to become agile and differentiate itself from others relies heavily on its capacity to foster innovation and to achieve and sustain a strong competitive position. Balanced Scorecards offer a holistic and detailed view of performance by framing strategic objectives within a balanced set of areas that contribute to the agency’s success and agility. They accelerate the process of embedding process improvement into every aspect of the organization so it becomes a central part of the culture.
Properly measuring KPIs and aligning tangible and intangible incentives at multiple levels of the organization to reinforce desired behaviors supports organizational agility as EMS deals with the ever-increasing pace of change.


