This feature is part of the 2018 EMS Trend Report, an in-depth look at EMS trends in the U.S. and an assessment of how the EMS profession is changing. To read all of the articles included in the 2018 report, click here.
By Guillermo Fuentes, MBA and Jay Fitch, PhD
EMS is at a critical juncture in its maturation, and it is the perception and attitude of those who work in the industry that will impact the future. Culture change can only happen if leaders recognize it’s needed, and the profession takes concerted efforts to make it happen.
This year marks the third annual EMS Trend Report, but the first time that the survey was open to any member of the profession. In addition, several new questions were added to gain a better understanding of where EMS personnel feel the profession is headed. Survey questions were developed by Fitch & Associates in collaboration with the EMS1 Editorial Advisory Board. A cross section of educators, EMS providers and EMS leaders vetted the questions prior to public release.
It is important to measure how EMS professionals feel about their field because it tells us a lot about which direction the profession is headed. No one knows EMS better than the people living it every day. Respondents were polled about facts, as well as their perceptions and opinions of the state of EMS in five different areas:
- State of the profession
- Safety
- Healthcare integration
- Finances
- Operations/clinical issues
The online survey was conducted in early 2018 and open for four weeks. Responses were received from 1,259 individuals from a diverse representation of communities, system models and years of EMS experience. As in the previous two years, the EMS Trend Report Cohort – leaders from the same group of agencies that will be polled each year – was asked to complete the survey. In most cases, the cohort members’ responses mirrored those of other respondents; at times it differed, as is noted throughout the report.
About the respondents
The EMS Trend Report survey was completed by EMS professionals in all 50 states, the District of Columbia and Puerto Rico. Respondents were predominantly male, field providers with 10 or more years of experience on the job. Responses came equally from urban, suburban and rural communities and were distributed across different service models.
EMS job satisfaction
Although EMS has changed throughout the years, one thing remains a constant – it’s about patient care and serving communities. And that continues to be what appeals to EMS providers, who cited patient interaction (62 percent) as the most satisfying aspect of their jobs. It’s critical that leaders in the profession keep this in mind as technologies, from electronic patient care report documentation to telemedicine, evolve and change how caregivers interact with the people they serve. Other top factors cited by respondents were community service (52 percent) and intellectual stimulation (37 percent).
Mixed optimism for the future of EMS
While optimism isn’t necessarily a predictor of good things to come, its presence in a culture, whether organizational or global, can be a catalyst for change. Shared optimism by a workforce is more likely to lead to embracing change rather than resisting it – which could be important if the many predicted changes expected in healthcare and EMS’ role come to fruition.
Nearly two-thirds of respondents expressed optimism about the future of EMS and a respondent’s role in their organization affected whether they shared those positive feelings. Only half of field providers reported being optimistic about the future of EMS, compared to much higher proportions of educators, supervisors and administrators.
Similarly, about a third of respondents said they wouldn’t recommend EMS as a career to a young person today. The reasons given were varied, and included stress, wear and tear on the body, low pay, limited career opportunities and a lack of respect from other medical providers.
Leaders certainly felt differently. A majority of the EMS Trend Report Cohort members were more likely to recommend EMS as a career, with only 16 percent saying they would not.
This difference in the degree of optimism reinforces the need for effective leadership, better communication and inclusive dialogue within all levels of an EMS organization, and the development of a shared vision of how EMS needs to evolve to best serve patients, communities and providers.
Community Paramedicine implementation
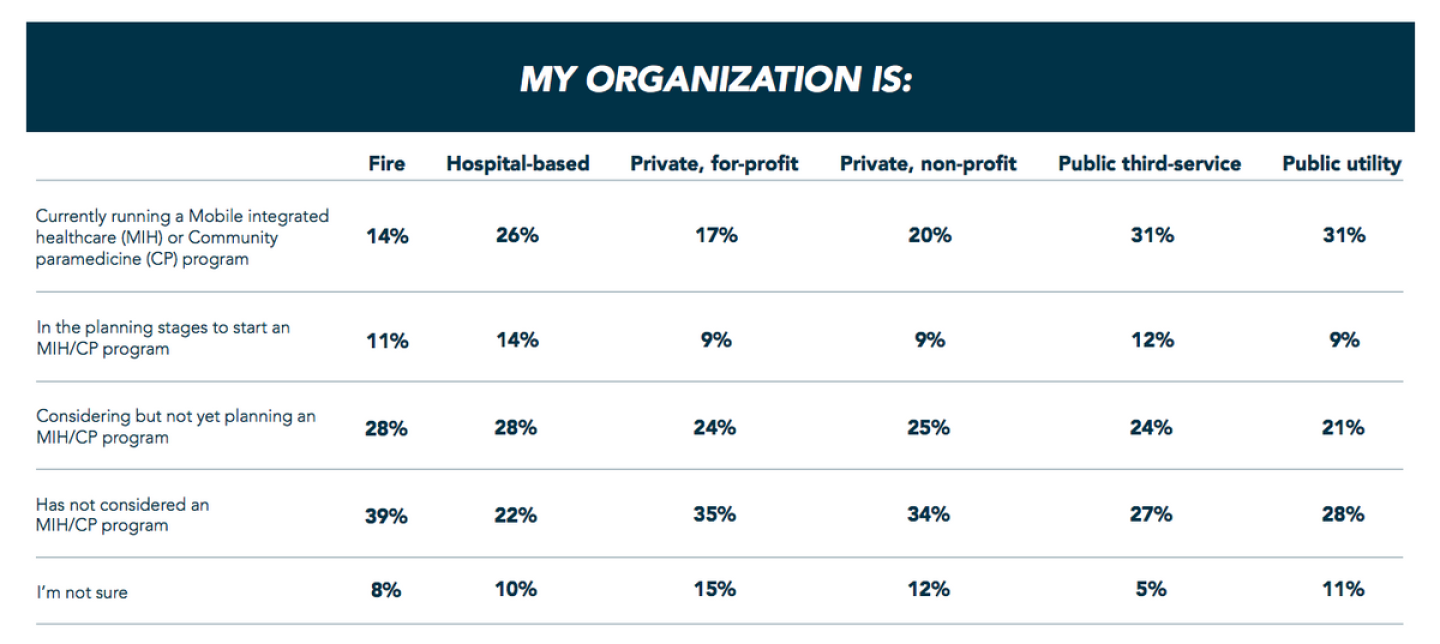
Most respondents agreed that innovative mobile integrated healthcare and community paramedicine programs (65 percent) are paving the way for the future of EMS. Not surprisingly, they also work for the most part in agencies that have already implemented or are considering MIH or CP programs. Public and hospital-based EMS agencies were most likely to have a program up and running, while private and fire-based EMS systems were more likely to be in the planning stages.
Surprisingly, though, respondents aren’t rushing to take the “emergency” out of EMS. Despite efforts by some membership and advocacy groups to promote the adoption of a new term for the profession, field providers largely rejected “paramedicine” or “mobile integrated healthcare” as names for their profession. Likewise, administrators and educators also leaned toward keeping the status quo.
While the number of medical director respondents to the survey was relatively small, the strong support (two-thirds) for retaining EMS may suggest a reluctance to broaden the mission so soon after EMS became recognized as its own medical subspecialty. Any proposed change in the name will require the support of this influential stakeholder group.
When looking by service model, both fire-based providers and those working for private, for-profit organizations strongly support the continued use of “EMS.” Respondents from hospital-based and public third-service agencies were the strongest supporters for use of “paramedicine,” which has been endorsed by the National EMS Management Association and an official advisory from the National EMS Advisory Council. Perhaps this is understandable, given the close affiliation these two service models have with healthcare or public health.
 While the debate over what to call EMS continues, it’s clear that most members of the profession feel the public doesn’t understand what they do (84 percent). Will changing our name help that or muddy the waters?
While the debate over what to call EMS continues, it’s clear that most members of the profession feel the public doesn’t understand what they do (84 percent). Will changing our name help that or muddy the waters?
Paramedic education requirements
The potential for paramedics to play a larger role in helping patients navigate the healthcare system, along with the growth of paramedic degree programs, has led some leaders and educators to call for increased education requirements.
Not surprisingly, support varies across different groups. Only 16 percent of respondents indicated a bachelor’s degree should be the minimum level of education for paramedics. Among respondents who identified themselves as primarily volunteer EMS providers, support for a bachelor’s degree was 11 percent, with nearly one-third of volunteers saying that a high school diploma was sufficient.
Recruiting and retention are top concerns
It’s likely the debate about increased education requirements is influenced by a sense across the industry that recruiting qualified EMS providers is already difficult.
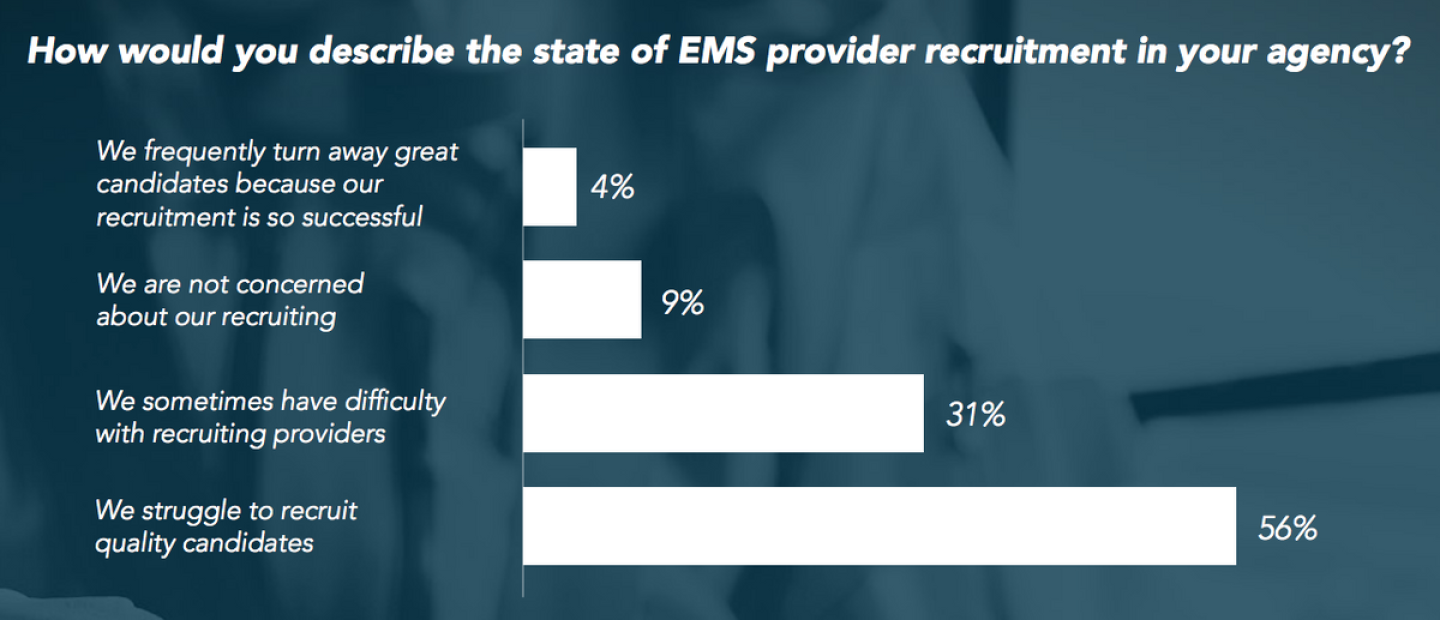
More than half of respondents said they struggle to recruit quality candidates to work as EMS providers in their organizations (56 percent). Nearly a third of the remaining respondents said they sometimes have difficulty recruiting EMS providers.
Importance of provider safety
The delivery of prehospital care is filled with potential risk for the provider and patient. For several years, national organizations have been pushing to improve safety, and many services have made great strides in areas such as seatbelt use, safer ambulances and patient movement devices, preventing medical errors and creating awareness around provider mental health issues.
However, a troubling disconnect appears to exist between leadership and providers as to whether their organizations are making patient and, especially, provider safety a priority. For example, while 92 percent of senior leadership thinks their organizations prioritize patient safety, 74 percent of field providers do.
For provider safety, the results are even more disparate. Only six percent of leaders said their organizations haven’t made provider safety a top concern, compared to 28 percent of field providers. Respondents who said they work for private, for-profit services were the least likely to agree that their organizations prioritize patient safety, provider safety and mental health.
There is a similar disparity between field providers and management when it comes to the prioritization of EMS provider mental health.
Addressing provider fatigue
Fatigue has long been a concern in EMS, where boasting about long shifts is often a rite of passage. Finally, there seems to be movement toward industry-wide recognition of the dangers posed by provider fatigue and finding ways to mitigate its impact on safety, patient care and caregiver health. The recent publication of evidence-based fatigue management guidelines, as well as additional research, is a step in the right direction. But most providers feel their organization is not addressing the problem, and even many in leadership positions acknowledge they are not tackling the issue.
Lights and sirens use
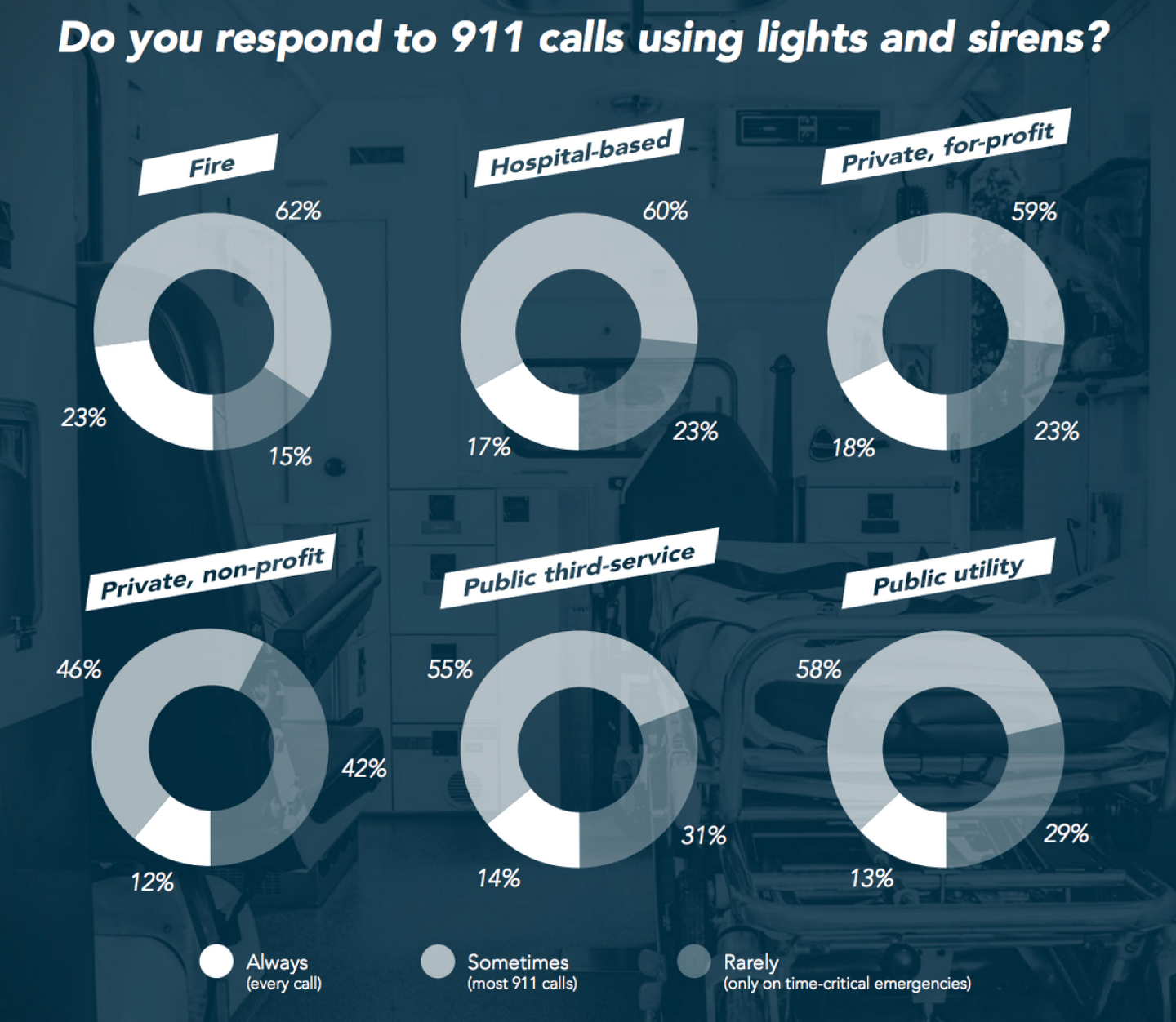
Although the number of agencies always using lights and sirens is relatively small, tradition in the fire service continues to prevail with 23 percent of respondents reporting use of lights and sirens for every call, compared to 17 percent overall. (The Cohort answered 27 percent with every call.) With research recently pointing out that the risks of using lights and sirens outweigh the benefits in the vast majority of EMS responses, watching this trend over the next several years will be revealing.
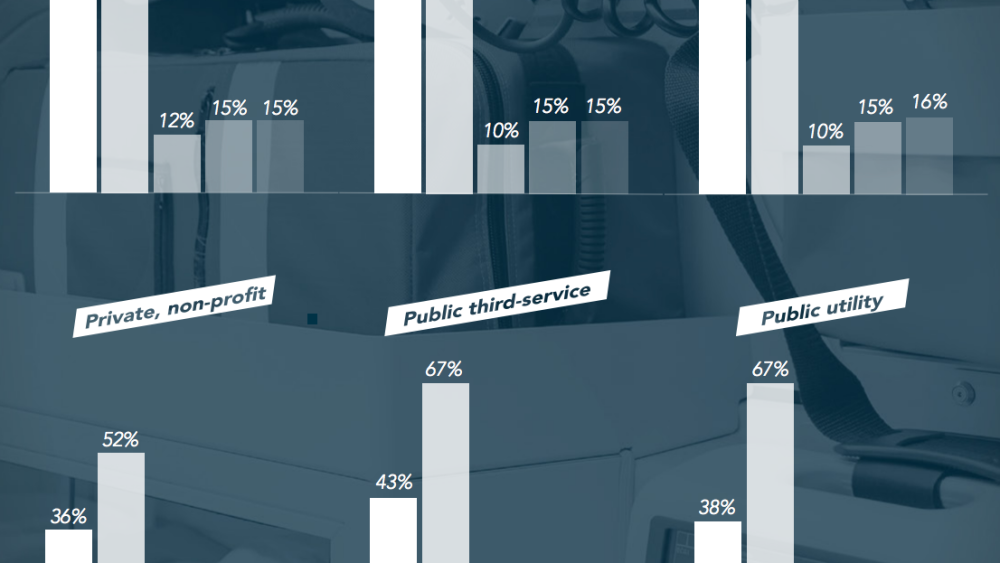
Making progress on healthcare integration
Better integration between EMS and the rest of healthcare may improve patient care, reduce costs to payers, improve the provider experience, potentially grow revenue and offer career advancement for EMS professionals. The survey suggests EMS systems are moving toward greater integration. More than two-thirds of respondents in leadership positions indicated integration with the rest of healthcare had improved in recent years. Noteworthy are public utility, third-service and hospital-based service models, which reported more recent improvement than other service types.
 Again, however, fewer field providers (61 percent) reported improvements in integration with the healthcare system. Are they not seeing the effects of better integration or are leaders not doing a great job of communicating improvements?
Again, however, fewer field providers (61 percent) reported improvements in integration with the healthcare system. Are they not seeing the effects of better integration or are leaders not doing a great job of communicating improvements?
Community education and public injury and illness prevention
The 1996 “EMS Agenda for the Future” called for prevention to be institutionalized into the mission of EMS as fire prevention is in the fire service. But the evidence suggests that while there are great examples of individual champions of prevention programs in a variety of agencies, it’s rare to see prevention memorialized into department budgets. Incentives and public expectations of EMS-led injury prevention are still not aligned.
Taking into account those who were neutral, only 6 percent of respondents disagree that community education and public injury and illness prevention should be a priority of EMS systems. Seven percent of the Cohort disagree. Eighty percent of respondents agree or strongly agree that education and prevention is an EMS provider and agency priority.
 Increasing budgets, finally
Increasing budgets, finally
The improving economy has increased tax revenues for most local, county and state jurisdictions. The survey results suggest that government-subsidized EMS services are benefitting, with respondents from fire and third-service systems reporting budget increases. Overall, more than half of those in administrative leadership positions said their organization’s budget has increased in the past year. The Cohort response was also strong, with 65 percent reporting a budget increase.
EMS reimbursement continuing concern
Reimbursement models for prehospital medical care have not changed significantly in many years, despite lobbying efforts to convince public and private insurers to fund preparedness efforts and pay for medical assessment and treatment, not simply transport.
After recruitment and retention, reimbursement was the third most reported concern of survey respondents. While the topic is complicated, one thing is certain, almost no one feels current reimbursement rates are adequate to cover the cost of providing EMS in their community.
Issues impacting the EMS profession
In this final section, we look at a variety of human resources, clinical and operational issues. More than half of respondents (61 percent) said provider mental health is a significant issue and violence against EMS providers was a major concern (42 percent) for all service models.
Equipment and technology
Future editions of the EMS Trend Report will help us follow developments and advancement in equipment and new technology being used in EMS. This year, it’s clear that while prehospital ultrasound continues to generate a lot of buzz, it’s still not being used by many services (4 percent). Induced hypothermia for cardiac arrest victims, once nearly universal until the most recent American Heart Association guidelines tempered the enthusiasm, is still being used by 19 percent of survey respondents, as compared to previous responses of the Cohort in 2017 (29 percent) and 2016 (38 percent).
Interestingly, 11 percent of respondents report their agencies are arranging alternative transportation methods, such as taxis or ride-shares. As more communities look for ways to reduce unnecessary costs and improve the patient and provider experience, use of alternative transportation methods has the potential to impact the finances of EMS organizations still relying on billing for transport to fund operations.
All-hazard preparedness
From influenza to hurricanes to active shooter incidents, the past year seemed to include an uptick in all types of major health emergencies, natural disasters and violent mass casualty incidents. When asked how prepared they felt their organizations were to respond to different types of disasters, field providers were skeptical, while leaders were more hopeful. In the case of nuclear incidents, however, almost no one feels very prepared, a possible sign that all-hazard preparedness for every type of disaster remains a challenge that EMS and all of public safety.
Medical director engagement
It is interesting to note the percentage of field providers who don’t believe their medical director is “very engaged” with them vs. the percentage of medical directors and other organizational leaders who believe they are engaged with field personnel. It’s important to note, a small number of medical directors responded to this survey, and it’s likely that those who participate in surveys about the state of EMS are more likely to be engaged with field providers.
Given that reality is perception, medical directors still have a long way to go if they want the paramedics, EMTs and medical first responders they work with to feel they’re adequately engaged.
EMS data and performance measurement
More than half of respondents agreed that they were “very satisfied” with the electronic patient care reporting software used by their system. Dissatisfaction was higher among field users (35 percent) than administrators (19 percent), which is not surprising given some comments noted that electronic charting was hurting provider’s ability to interact with patients.
In general, attitudes toward electronic charting seem to be improving which is possibly the result of a growing proportion of the workforce that has never known paper charting, grew up using computers and understands the benefits of data sharing and analysis.
At the same time, it seems many respondents are unfamiliar with the role that the National EMS Information System has played in shaping those electronic systems. When asked whether NEMSIS has contributed to the advancement of EMS, more than a third agreed, but even more said they “don’t know.” Even among leadership, about 25 percent of respondents said they weren’t sure, while about half of chiefs and administrators felt NEMSIS had made a positive difference.
One struggle for EMS systems continues to be accessing outcome data for patients they transport to hospitals. Even for cardiac arrest victims – typically a small number of patients – only 42 percent of respondents said their organizations track patient survival-to-discharge. An even smaller number (14 percent) looks at cerebral performance category score, which is a measure of whether the cardiac arrest survivor was able to return to a productive lifestyle.
Most respondents (62 percent) said their agency continues to measure return of spontaneous circulation, even though some studies have indicated interventions that improve ROSC, such as epinephrine, may actually decrease the chances of survival-to-discharge.
Many respondents (27 percent) weren’t sure if their organization tracks cardiac arrest data, which is a potential indication that systems either aren’t measuring performance or are not adequately sharing the numbers with the providers performing resuscitations. Sharing and explaining results with the providers who are essential to improving system performance.
Conclusion
While the 2018 EMS Trend Report examined a range of diverse EMS topics, some common themes emerged. Perhaps most striking was the perception gap between administrators and providers. They often disagreed on whether their organizations’ efforts to tackle issues such as provider mental health and provider safety were sufficient.
While it may not be surprising that these two groups don’t always see eye-to-eye, the results do point to the need for increased communication between leadership and staff. Taking a proactive approach and surveying – either formally or informally – your own field providers, support staff and leadership can let you know if these disconnects exist in your organization.
Increasing communication will also help improve your agency’s ability to retain reliable, talented personnel. From large metropolitan departments to rural volunteer organizations a lack of communication between leadership, managers and field providers can decimate job satisfaction. Actively striving to increase levels of employee engagement can help retention, and even recruitment, as your current members are your best recruiters.
The 2018 EMS Trend Report results – a measurement of attitudes, perceptions and practices at this moment – should shape efforts to improve patient outcomes and help our communities. Only by looking at where we are now, deciding where we want to be, and deliberately taking the steps to get there, will EMS adapt, innovate and thrive in the future.
About the authors
Jay Fitch, PhD, is a founding partner of Fitch & Associates, and has spent more than four decades serving the EMS community as a leader, author, speaker, educator and consultant. Guillermo Fuentes, MBA, is the Fitch & Associates partner specializing in communications and technology. He previously served in operations and leadership roles in public safety in Montreal and the Niagara region of Ontario.
Acknowledgments
Fitch & Associates recognizes the contribution of Michael Gerber, Gigi DeWeese and Keith Griffiths of the RedFlash Group in the development of the report. We also appreciate the work of Geoff and Melanie Cady, in managing, sorting and analyzing the data. Geoff Cady is a former paramedic and EMS/fire consultant who has a strong history of using data in his engagements.